5 Hidden Dangers of Common Medications
May 20th 2016
By:

But OTC drugs come with reams of tiny warning text for a reason: Used under the wrong circumstances or in the wrong combinations, they can make you sick, damage your organs, or even kill you.
This isn't to say that OTC drugs are a public health hazard; in fact, they're a great first line of defense against everyday injuries and disease symptoms, according to Mohamed A. Jalloh, an Omaha-based Walgreens pharmacist who serves as a post-doctoral fellow of evidence-based medicine at Creighton University and a spokesman for the American Pharmacists Association.
"[Over-the-counter drugs] empower people to take control of their health and make it easy for people to get medications that will be helpful," Jalloh said. "If people have pain, they can get something from the pharmacy right away instead of having to wait for hours at a doctor's office or the hospital, and that's a great thing for most people."
The dangers of OTC medicines, Jalloh said, come into play when people don't talk to their pharmacists — or at the very least, pay attention to warning labels — to learn about dosing instructions and potential side effects or interactions.
ATTN: spoke with Jalloh by phone to learn about five of the most common hidden dangers associated with everyday over-the-counter drugs.
1. Tylenol can really mess up your liver
 Katy Warner/Flickr
Katy Warner/FlickrAcetaminophen is "a good medication that treats pain effectively," Jalloh said. But people need to take the dosing restrictions seriously. Pharmacists recommend that consumers take no more than 4 grams of acetaminophen in a day, "with caution," Jalloh said. That amounts to eight Tylenol Extra-Strength (500 mg) tablets in a day, and no more.
People have experienced liver toxicity in cases where they took even less than 4 grams, Jalloh said. A daily limit of 3 grams — the maximum dose that Tylenol recommends — can help consumers err on the side of caution.
One of the reasons that acetaminophen poses a special overdose risk is its pervasive presence in all manner of OTC cold and pain-relief products, Jalloh said.
"One thing you’ll see with a lot of these combination products, like DayQuil Multi-Symptom —they have acetominophen in it, and people aren’t aware of that, so they’ll take Tylenol as well," Jalloh said. "That’s an easy way to accidentally overdose."
Jalloh added that consumers should take seriously the oft-repeated warning to avoid mixing acetaminophen with booze.
"Both alcohol and Tylenol can cause liver toxicity individually," he said. "When you combine them together, it just makes it that much easier for your body to have liver damage."
2. Advil and Aleve can make your intestines and kidneys bleed
 Back pain/YouTube
Back pain/YouTube
Ibuprofen, the active ingredient in Advil, and naproxen sodium, the agent in Aleve, both fall under the category of non-steroidal anti-inflammatory drugs, or NSAIDs. While NSAIDs relieve pain in a slightly different way from acetaminophen and can help reduce inflammation, they share some similar dangers.
Too much of either type of drug can cause problems. In the case of NSAIDs, they can cause tissue damage and bleeding in your gastrointestinal system and kidneys, Jalloh said.
"[The guidelines] are really stringent as to how much [Advil or Aleve] you should take," he said. "And with NSAIDs, you get the same problem as Tylenol — a lot of combination products have them, so people will take Advil Cold & Sinus and then forget it has ibuprofen, so then they take ibuprofen in addition."
 frankieleon/Flickr
frankieleon/Flickr
Pharmacists recommend no more than 1,200 mg of over-the-counter ibuprofen in a day, which is equivalent to six 200 mg Advil tablets, Jalloh said. They recommend no more than 660 mg daily of naproxen sodium, which equals three 220 mg tablets of Aleve.
Because these drugs work in the same way and have similar GI effects, Jalloh added, doubling up on them is a bad idea: If you take the maximum daily dose of both drugs, you've "definitely" increased your risk of GI and kidney damage, he said.
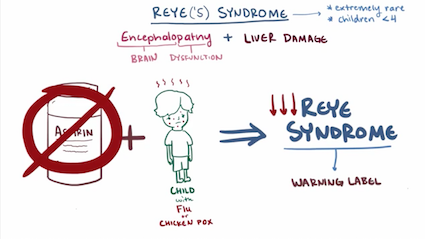
3. Aspirin may cause a fatal condition in children and teenagers
 Mike Steele/Flickr
Mike Steele/Flickr
Those who saw the 2015 Johnny Depp gangster biopic "Black Mass" might remember the devastating scene in which Depp's character, James "Whitey" Bulger, loses his 6-year-old son during a routine hospital visit due to a bad reaction to aspirin.
Not only is this is a true story, the danger that aspirin poses to young people is also very real, based on available evidence, Jalloh said. Aspirin can cause a rare condition in children and teenagers called Reye's Syndrome, which causes swelling in the liver and brain. This condition most commonly affects children between the ages of 4 and 12 who are recovering from a viral infection, like the flu or chicken pox.
"It can be really deadly," Jalloh said. "[Aspirin use] is not recommended at all for people under the age of 18. It’s one of those medications where people feel really comfortable with it, and it’s used to protect the heart, but young patients can quickly experience brain damage and liver function problems."
 Osmosis/YouTube
Osmosis/YouTube
The link between aspirin and Reye's Syndrome is a topic of ongoing debate, and other practitioners might give different advice, but Jalloh said that he stands by the recommendation that parents should avoid giving aspirin to children until well-controlled studies demonstrate that it's safe.
4. NyQuil can cause confusion in older people
NyQuil is famous for its hypnotic sleep-inducing powers — as well as the dreaded "NyQuil hangover" some people get the morning after.
The risks of NyQuil and other medications that contain antihistamines that make you sleepy — doxylamine in the case of NyQuil, diphenhydramine in other cold and allergy medicines like Benadryl — go beyond abusing your "snooze" button, though, or even the label warning that these drugs can impair your ability to drive and operate machinery.
Jalloh said that these medicines fall under a classification called the Beers Critera or Beers List, established by the American Geriatrics Society. That means they may not be appropriate for patients older than 65.
In the case of NyQuil and other OTC products that induce drowsiness, they can cause elderly patients to become confused, seemingly out of the blue, Jalloh said.
"These types of medications can increase the risk of confusion in older patients," he said. "There doesn't have to be any history of dementia or anything like that — it can happen to any older person."
5. Long-term Nexium or Prilosec use might cause a host of health problems
 Mike Mozart/Flickr
Mike Mozart/Flickr
Proton pump inhibitors like Prilosec and Nexium, which shut off the production of stomach acid, have soared in popularity over the past decade or so — perhaps thanks to marketing efforts that portray them as a "magic bullet" for heartburn. A 2009 study found that PPIs were the third most commonly used type of drug in the United States, and Nexium has even acquired the nickname "purple crack" among some doctors and long-term users for its addictive qualities.
Unfortunately, despite Larry the Cable Guy's promises, you can't just pop Prilosec and eat whatever you want without consequences, Jalloh said. A number of recent studies have linked long-term PPI use with serious health problems. But many patients continue to stay on these drugs for years at a time, unaware of the mounting evidence against them, Jalloh said.
 GIFsoup
GIFsoup
"There are so many studies coming out that [long-term PPI use] is associated with kidney damage, heart attacks, bone fractures, dementia — even people dying," Jalloh said.
The best thing PPI users can do is talk to their doctor and make sure it's still necessary to keep up PPI treatment. For many of these patients, a step down to plain old Tums could treat their symptoms adequately.
"My concern is that a lot of people are taking [PPIs], and they had a legitimate reason at one time — maybe they had gastroesophageal reflux disease — but typically you're only directed to take it for a certain amount of time," Jalloh said. "Instead, people are taking it just to keep doing it, and they don't need to because it’s already served its purpose."


No comments:
Post a Comment